
One obstacle to diagnosis of sleep apnea is patient fear of treatment options. They may not know that patient-centric options are available.
Read More
Once you have the right strategies in mind to tackle healthy eating and take action to follow them, staying healthy becomes easier over time.
Read More
Doctors are often frustrated by patients who don’t follow their weight loss advice. Here are 5 reasons why patients may ignore it.
Read More
Eating disorders are among the most dangerous and difficult to treat of all mental health disorders. Here is what you need to know about them
Read More
Severe eating disorders may be accompanied by life-threatening medical complications that require stabilization before psychiatric treatment.
Read More
Body dysmorphic disorder is a syndrome in which a person can’t stop thinking about some perceived flaw in their appearance.
Read More
We all have our favorite excuse for not exercising. However, many of them do not hold up to scrutiny. Here are 12 commons exercise excuses, debunked.
Read More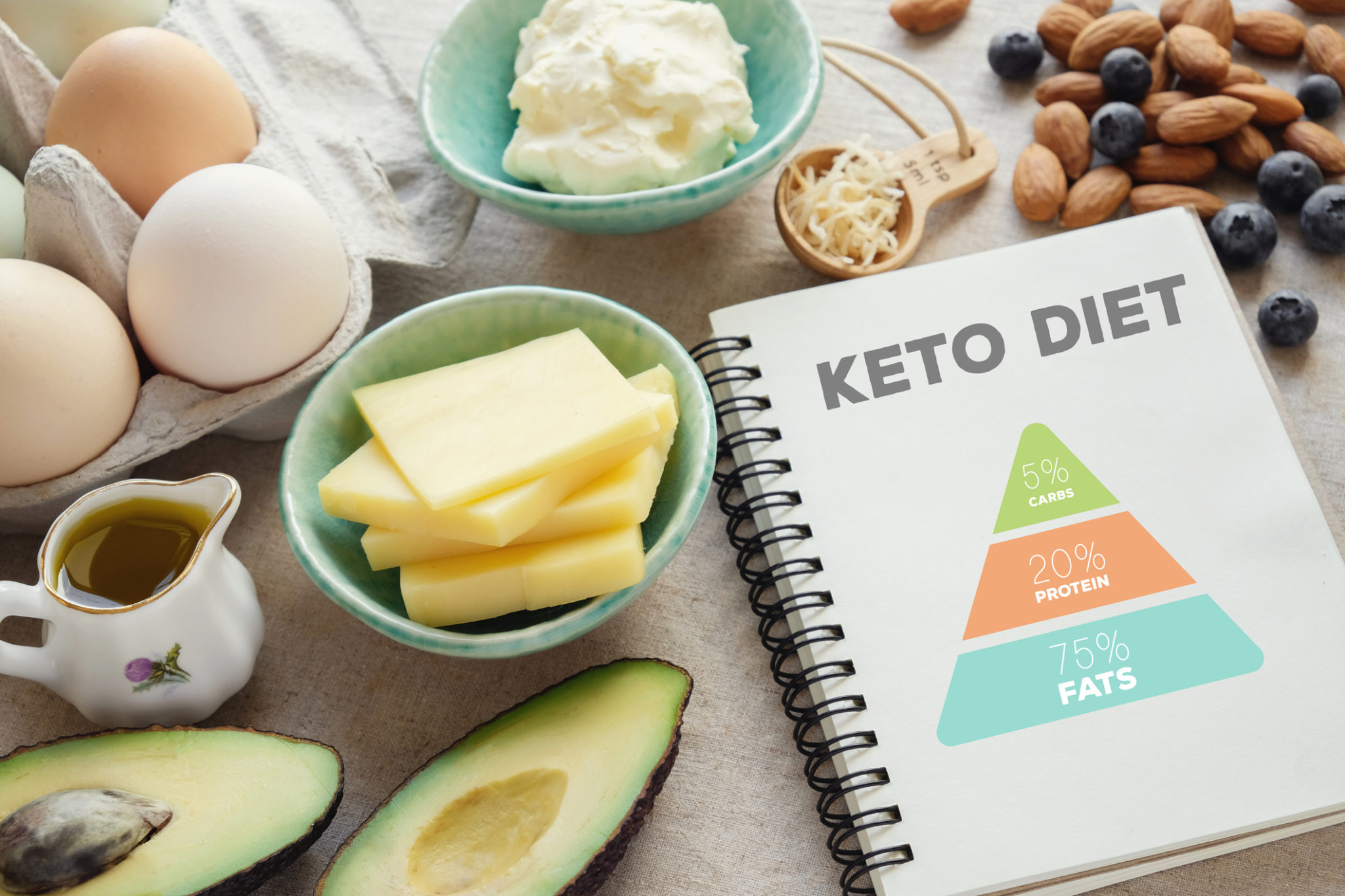
The keto diet is a low carb, high fat, moderate protein diet that forces the body to burn fats for energy creating ketosis. It’s effective for weight loss.
Read More
Getting your children to play outside isn’t just for fun, it’s good for their growing bodies and minds. Here are some simple, fun activities they will love.
Read More
There are certain benefits of riding a bike that driving a car could never live up to. Here are 5 reasons to hang up your car keys.
Read More
Are carbohydrates necessary for workout recovery or can a fat-fuel diet be just as good?
Read More
We’ve all heard the old adage, ‘no pain, no gain’, when it comes to exercise but could this phrase be doing more harm than good?
Read More