
The orderly progression of cases in the OR is interrupted when an l-year-old is rushed in, mottled and limp, from a pediatric airway emergency
Read More
Comprehensive eye exams do more than check if you need new glasses. They also include tests for eye diseases. And, they may detect some chronic diseases.
Read More
A medical student learns about empathy from a busy pediatrician who advised her that learning from patients’ stories can be more important than giving medications.
Read More
The common, annoying conditions of dandruff and seborrheic dermatitis are conditions that involve an increased rate of shedding of the topmost layer of the skin called the epidermis.
Read More
Prenatal exposure to toxic chemicals is linked to preterm birth, birth defects, childhood cancer, obesity, diabetes, asthma, & lasting harm to the brain. SafetyNEST, a startup whose mission is to be the most trusted source for pregnant women & their healthcare providers, helps safeguard babies’ against everyday toxic chemicals.
Read More
As the obesity epidemic continues to grow, we are seeing serious complications, including non-alcohol fatty liver disease (NAFLD), in many obese people, including very young children. In some cases, the damage to the liver leads to irreversible scarring requiring transplantation. If diagnosed and treated early, these complications can be prevented.
Read More
A highly publicized death of a child due to a rare form of drowning, terrified parents needlessly. Here’s what you need to know about secondary and dry drowning.
Read More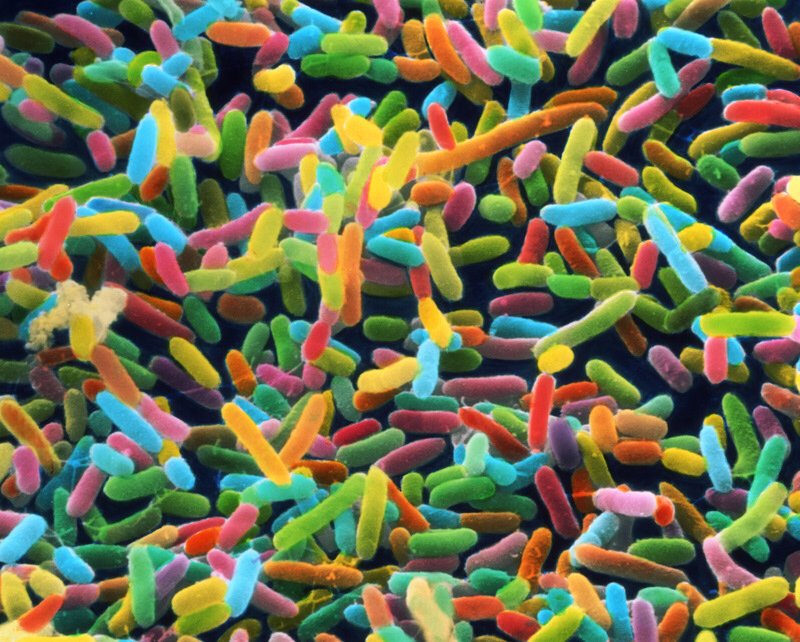
Most parents (and even some doctors) are unaware of the critical role of the infant microbiome as a foundation for good health throughout a child’s life.
Read More
Brain development has been shown to benefit from free play, where children use their creativity and own ideas to come up with a desired game or type of play.
Read More
6-year-old Caleb Sears died while under general anesthesia for a dental procedure. His oral surgeon was both operator and anesthesia monitor, a practice many believe increases the risk of dental anesthesia. A California bill, known as Caleb’s law aims to decrease that risk.
Read More