Now and then, a solution emerges for a large, seemingly insurmountable problem. In some instances, progress results when someone looks at a challenge with fresh eyes and sees a fix that wasn’t obvious before. More often, significant progress is born from a sustained history of incremental successes that, at some point, become a powerfully capable solution. This article describes one such solution, MedsEngine, that, in our opinion, has allowed chronic condition management to take a giant leap.
New Dr. Alisa Niksch‘s Review Notes appear at the end of the story.
One of Healthcare’s Biggest Challenges: Chronic Condition Management
One of healthcare’s biggest challenges is better management of major chronic conditions, including hypertension, diabetes, heart failure, and asthma, among others.
In 2016, chronic conditions and the downstream health and productivity events they generate consumed almost one-fifth of US Gross Domestic Product.1 These include (but are not limited to) direct medical costs for increased heart attacks, strokes, amputations, emergency visits, and hospital admissions, as well as indirect employer and patients costs like absenteeism.
In addition, University of California researchers have reported2 that the U.S. spends over half a trillion dollars per year in additional costs because chronic disease patients are being prescribed the wrong drugs. This class of conditions represents our most important health care outpatient improvement opportunity.
Related Content: Teens and the Challenge of Living with Chronic Illness
Meager Results from Chronic Condition Management Efforts
Efforts to manage chronic conditions have yielded despairingly weak results. Historically, measures of success have been expressed by the percentage of cases that are “controlled,” meaning patients’ metrics are within accepted limits.
Currently, only 44% of Americans with hypertension are controlled.3 Fewer than 10% of diabetics are controlled when their blood glucose, blood pressure, and cholesterol goals are considered.4 Among heart failure patients with reduced ejection fraction, only 1.1% are on all three of the most essential drugs and at effective doses as necessary to prevent further destruction of the heart muscle.5 Better control would translate to better health outcomes, fewer high-cost events, and lower overall costs.
The Usual Excuses for Poor Outcomes
The standard responses to poor results have been to assign blame. You’ve probably heard these excuses about why performance was subpar:
-
-
- Patients are not compliant about taking their medications.
- Doctors don’t give patients the attention they need.
- Chronic conditions are simply too resistant to control.
-
With these assumptions as a backdrop, most interventions aim to change patient behavior, typically with little success.
Two Essential Management Elements
These reactions ignore the complex structure of chronic diseases and what it takes to manage that complexity. As it turns out, two elements are necessary for successful chronic condition management:
-
-
- Physicians must prescribe the right medications for each patient.
- Patients must be engaged, participating in self-care, including taking their medications and lifestyle accommodations as required for their condition(s).
-
Let’s put aside the second, on the assumption that the right drugs deliver superior health outcomes, a reward that should easily win patients’ buy-in.
Insight: Choosing the Right Chronic Condition Therapy is Complicated
MediSync is a firm that develops and provides management services and solutions for large, high-performing primary care and multi-specialty physician practices. Over the past two decades, it sought to develop a software application for real-world medical groups. The MedsEngine application was designed to achieve nation-leading outcomes in major chronic diseases. While many provider organizations have a “blame the patient” analysis of poor chronic outcomes, MediSync’s root cause analysis led them to undertake a different approach.
The insight behind MedsEngine is that drug selection choices are more complicated than most prescribers recognize. And, physicians and Advanced Practice Providers (APPs) can achieve superior outcomes if they have access to expert assistance in evaluating and selecting the individual patients’ precise medications.
–The number of variables is quite large
The number of variables involved in choosing optimal medical therapies generates millions of permutations. For example, there are five distinct hemodynamic causes for hypertension. MediSync has further identified several dozen demographic factors (i.e. age, race) and comorbid conditions, each of which could change the optimal medication choices.
MediSync also recognizes twelve different drug classes – with multiple drugs within each class – to improve hypertension outcomes. The problem is that most physicians are comfortable using no more than five or six drug classes, and many patients require two or more classes of antihypertensive drugs, making the permutations even more complicated.
–Complex Calculations are Best Done by Computers
Most other professions have come to appreciate that extremely complex calculations are best done by computers. The complexity associated with juggling multiple variables can exceed humans’ capacity to rely on memory and mental calculation.
In the end, few physicians working without an aid like the MedsEngine prescribe the best medications. And, not surprisingly, few of their patients achieve safe blood pressure levels, as reflected in the national 44% success rate in successfully managing high blood pressure.
Artificial Intelligence (AI) is Required to Handle a Large Number of Variables
Artificial Intelligence (AI) is an optimal solution for this type of challenge. When properly designed, it can capably and reliably handle large numbers of variables. That approach, when applied to the complexity of chronic condition management, has been MediSync’s vision.
MediSync’s chronic disease management improvement project began 20 years ago, with the realization that making the right drug choices is an impediment to improved outcomes. Working at that time in paper medical records, it developed a first generation of “paper and pencil” decision support tools to drive better medication selection. Piloted by PriMED, a progressive, 55-physician, independent primary care practice based in Dayton, OH, by 2007 this approach resulted in 93% group-wide success (BP <130/80 for hypertension with renal dysfunction or diabetes; <140/90 for all other patients) across the practice’s entire population of hypertension patients. When compared to the CDC “success rate” of 48%, this was a remarkable outcome (Table 1).
 Moving to a Cloud-Based Solution
Moving to a Cloud-Based Solution
But as the number and complications of diagnoses grew, paper and pencil tools became increasingly problematic. In 2016, MediSync began to develop the MedsEngine, an AI-driven tool that deploys complex, mathematical algorithms reflecting the best current understanding of each chronic disease’s physiology and pharmacology, and the relevant interactions occurring among and between them.
Pulling patient information from the electronic health record, the MedsEngine performs several, sequential calculations. First, it calculates the hemodynamic forces that drive each specific patient’s blood pressure problem, including problems in the blood vessels, heart problems, fluid problems, or combinations of these underlying issues.
♦♦Love Our Content?♦♦
Sign up for our Newsletter Here
Second, the MedsEngine considers 28 comorbid conditions that, when present, can influence which classes of drugs may be contra-indicated and which may be promoted or demoted. It also addresses whether there should be a change in the order of drugs prescribed for patients who require multiple classes to gain blood pressure control.
Related Content: Artificial Intelligence: Can It Improve Results of Cancer Screening Programs?
In 2017, MediSync initiated a MedsEngine pilot with PriMED. The group’s hypertension results improved to their highest degree ever, averaging between 93% and 95% of all hypertension patients in good control each month (Table 2).
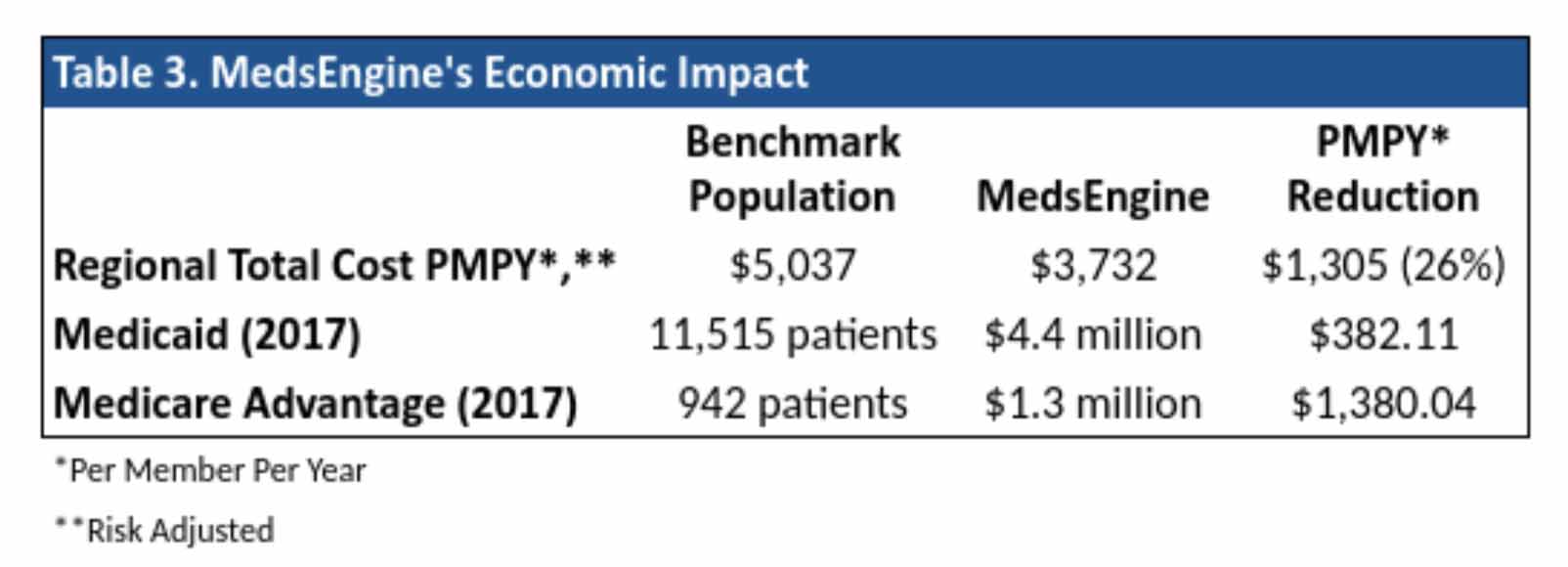
 Since hypertension, cholesterol, diabetes, and the other, most common chronic diseases cause many of the higher cost events like heart attacks, strokes, kidney damage, amputations, ER visits, admissions, and readmissions, PriMED expected to see significant reductions in the total cost of care for its patients. The data strongly supported that better chronic outcomes result in lower costs of care as Table 3 below demonstrates:
Since hypertension, cholesterol, diabetes, and the other, most common chronic diseases cause many of the higher cost events like heart attacks, strokes, kidney damage, amputations, ER visits, admissions, and readmissions, PriMED expected to see significant reductions in the total cost of care for its patients. The data strongly supported that better chronic outcomes result in lower costs of care as Table 3 below demonstrates:
 MedEngine’s Validated Performance
MedEngine’s Validated Performance
This performance improvement has been validated and recognized by credible third-party groups. The American Medical Group Association (AMGA) ranked PriMED best in the US at achieving blood pressure outcomes of ≤140/90 mm Hg with 95% of their hypertension population under control.7 Similarly, the Centers for Disease Control certified PriMED as first in their Million Hearts awards program.7 It is the only large group nationally to exceed 90% of hypertension patients under control.
The same technology drove PriMED’s control of Type 2 diabetes. This program was also recognized by AMGA as first among US physician groups, achieving simultaneous control of all three major Type 2 diabetes markers: blood pressure, LDL, and HbA1c.
When Chronic Diseases are Controlled, There are Clinical and Financial Impacts
Within the past few years, various federal laws and rules have required that larger physician groups must measure their blood pressure control success rates. During that period, overall blood pressure control rates have declined, not improved. The ability to predictably control the major chronic diseases is a significant advance, with important clinical and financial impacts to the patient and to the US health system.
A system that allows providers to reliably achieve performance targets enhances patient care and value. Importantly, it also allows those providers to optimize health outcomes and savings. This makes them far more desirable in a value-focused marketplace. In other words, the MedsEngine can serve as a foundation for care that is more evidence-based, accountable, and predictable.
The MedsEngine’s AI-driven platform capabilities are already established for three major chronic conditions:
-
-
- Hypertension
- HFrEF (heart failure with reduced ejection fraction)
- Hyperlipidemia
-
And, the diabetes program is currently underway. Furthermore, MediSync intends to complete clinical decision support platforms for the top 12 chronic diseases addressed in primary care within three years. They include:
-
-
- Hypertension
- Diabetes
- Dyslipidemia
- Coronary artery disease and peripheral vascular disease
- Chronic kidney disease
- Heart failure
- Chronic obstructive pulmonary disease
- Asthma
- Depression
- Anxiety
- Osteoporosis
- Arthritis
-
The Bottom Line for Chronic Condition Management
Mark DeRubeis, CEO of Premier Physicians in Pittsburgh, the other MedsEngine pilot site, summed up the promise represented by this approach:
“The MedsEngine offers the opportunity for exponential improvement in chronic care management. It enables you to get the diagnosis right the first time, to prescribe the right medicine the first time. If you look at the alternative to that, it may take two or three or four times the effort, and this enables you to cut all of that out and gain an efficiency that didn’t exist prior.”
US health care reimbursement is still dominated by fee-for-service, which has been rewarded by overtreatment and so favors more, higher cost care. Value-focused arrangements that reward better health outcomes and/or lower costs are now gaining accelerating traction in the marketplace. However, for high-value vendors, progress may feel glacial.
High-value approaches like the MedsEngine are gradually being embraced by organizations at financial risk for their health care costs – e.g., employers, third party administrators, stop-loss carriers, providers in risk-based arrangements, Medicare Advantage and Managed Medicaid plans – but acceptance at this point remains an uphill battle.
The MedsEngine is the first of what will almost certainly be a flood of new digital tools that facilitate far more effective care. It was built and is continuously updated using the best current established evidence so that clinicians can feel confident in the process. It offers a highly refined, mechanized way to leverage the best guidance from the management of complex inputs. However, building these tools well is as complicated as the problems they seek to address. Fortunately, the rewards, in terms of better health and lower costs, are likely to be equally powerful.
References
- Waters H, Graf M. The Cost of Chronic Disease in the U.S., Milken Institute, 2018 Aug. https://milkeninstitute.org/sites/default/files/reports-pdf/ChronicDiseases-HighRes-FINAL.pdf
- Watanabe JH, McInnis T, Hirsch JD. Cost of Prescription Drug–Related Morbidity and Mortality. Annals of Pharmacotherapy. 2018;52(9):829-837. doi:1177/1060028018765159.
- Munter P, Hardy S, Fine L, et al. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999-2000 to 2017-2018, JAMA 2020;324(12):1190-1200. doi:10.1001/jama.2020.14545 https://jamanetwork.com/journals/jama/article-abstract/2770254?
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
- Greene S, Butler J, Albert N, et al. Medical Therapy for Heart Failure With Reduced Ejection Fraction: The CHAMP-HF Registry, J Am Coll Cardiol, 2018 Jul 24;72(4):351-366. DOI: 1016/j.jacc.2018.04.070
- T2G Goal Post. The Monthly Newsletter of National Together 2 Goal Campaign, March 2018 edition. httpss://together2goal.org/assets/GoalPost/1803.html
- PrimeMed Press Release, Feb. 2015. https://www.primedphysicians.com/content/documents/PriMed-Media-Hypertension-Success.pdf
Keywords: chronic condition, chronic disease management, artificial intelligence, hypertension, diabetes, heart failure, MedsEngine, primary care, better health outcomes, cost savings.
Financial disclosure: Both Brian Klepper and John Rodis, M.D. have consulting relationships with MediSynch, the parent company of MedsEngine.
Medical Reviewer Notes by Dr. Alisa Niksch
MedsEngine exemplifies the potential of AI in the healthcare industry and the very real need for automation to reduce inefficiencies of the traditional trial and error process.
There are an enormous number of AI tools for clinical decision support which have entered the healthcare market over the last 5 years. Many of them are comprised of fairly transparent algorithms aggregating different data sets to generate an output that can guide management. In this case, an initial goal was optimal medical therapy for hypertension. The MediSync team made the smart decision to trial their algorithms in a real clinical setting.
An early partnership with clinicians who can provide a real-world test for the software, both from clinical results and workflow standpoint, is incredibly valuable. However, it is still elusive what disclaimers surround the use of the software, what percentage of recommendations made by the MedsEngine software were followed, and despite published cost comparisons, whether other patient experience was affected (e.g. increased drug costs, prior authorization denials).
While pilot studies can yield impressive results for clinical outcomes, AI must be evaluated in ethnically and geographically diverse populations to determine its ability to generate similar results on a large scale.
In fact, this is a principle the FDA requires for evaluating clinical trial data submitted in support of a 510K application – especially if there is a machine learning component to the software.
In this case, an AI platform that provides personalized treatment plans with specific drug recommendations may fit into the category of software as a medical device (SaMD). Regulatory processes provide risk mitigation and correction of any vulnerabilities which may lead to errors or misuse which could potentially harm patients. When innovators are looking to design AI platforms that inform, drive, diagnose, or treat medical conditions, evaluating a regulatory strategy with appropriate validating data is key to success.
Brian Klepper Ph.D. and John Rodis, M.D.
Brian Klepper, Ph.D. is a Principal of Worksite Health Advisors and a nationally prominent health care analyst and commentator. He speaks, writes, and advises extensively on high-performance health care, primary care clinics, and the management of clinical and financial risk.
A purchaser advocate, he has focused on the market and policy dynamics of the health care cost crisis and readily available solutions to purchasers willing to approach the problem laterally. His current focus is on high performing health care organizations that consistently deliver better health outcomes at a lower cost than conventional approaches in high-value niches.
Dr. Klepper has been involved in several transformative health care efforts favoring patient and health care purchaser interests. His 2009 testimony to an HHS panel resulted in the revocation of an industry group’s monopoly on Health Information Technology certification. In 2010-2013, he spearheaded a national effort, culminating in a lawsuit against CMS and HHS, to expose the AMA’s RBRVS Update Committee’s role in distorting US’ care and cost patterns.
Brian is a regular contributor to the health care trade press. He is a reviewer for the journals Health Affairs and The Journal of Ambulatory Care Management, and an advisor to several health care organizations. He is the Founder and Moderator of The Healthcare Benefits Hackers listserv, a vibrant discussion forum with 850+ participants focused on health care value and high performance.
George Washington University’s Masters in Health Administration Program ranked Brian's writing, archived at Care & Cost, the top 2016 blog by a health care professional. Feedspot named it a 2017 top 100 health care blog.
In his spare time, Brian is an offshore sailor.
John F. Rodis, M.D., M.B.A., is the founder and president of Arista Health, LLC, driving quality, safety, and patient experience and reduce risk in hospitals and health systems. He served as president of Saint Francis Hospital from 2015-2020, the eighth leader of Saint Francis and the first physician to serve as president since its founding in 1897. Dr. Rodis previously served as Saint Francis’ Executive Vice President and Chief Operating Officer, Chief Physician Executive. Prior to his executive leadership roles, Dr. Rodis served as Chairman of the Department of Obstetrics and Gynecology and Physician Leader of the Women and Infants Service Line, a position he assumed in 2011.
Under Dr. Rodis’ leadership, Saint Francis, a 617-bed major teaching hospital, the largest Catholic hospital in New England, earned its Level 1 Trauma Designation, opened its Smilow Cancer Hospital at Saint Francis and the Karl J. Krapek Comprehensive Women’s Health Center. During his tenure as president, the hospital garnered numerous awards and recognition including the 2018 and 2019 Women’s Choice Award® as one of America’s 100 Best Hospitals for Patient Experience, was named as one of the nation’s 100 Top Hospitals by IBM Watson Health™ and one of the World’s 1000 Best Hospitals by Newsweek. Moreover, the hospital recently attained its fourth consecutive “A” for Patient Safety from the Leapfrog Group, its seventh A in the last four years.
Before joining Saint Francis, Dr. Rodis served as Senior Vice President for Medical Affairs and Chief Medical Officer at Stamford Hospital, where he also previously held the position of Chairman of the Department of Obstetrics and Gynecology. Prior to that, he was at the University of Connecticut Health Center, where he was the Obstetrics and Gynecology Residency Program Director, a member of the Division of Maternal-Fetal Medicine and Director of Perinatal Genetics.
Dr. Rodis received his medical degree from the Autonomous University of Guadalajara, Guadalajara, Mexico. He completed his residency in obstetrics and gynecology at St. Joseph’s Hospital and Medical Center, Paterson, NJ. He completed fellowships in Maternal-Fetal Medicine and Clinical Genetics at the University of Connecticut Health Center. He also received his Master of Business Administration from Rensselaer Polytechnic Institute.
He holds the rank of Professor of Obstetrics and Gynecology at both the University of Connecticut School of Medicine as well as the Frank H. Netter MD School of Medicine at Quinnipiac University. He has attained a Black Belt in Lean Daily Management.
Dr. Rodis is Board certified in Obstetrics and Gynecology and Maternal-Fetal Medicine. He is a Fellow of the American College of Obstetrics and Gynecology, and a member of the Society for Maternal-Fetal Medicine and is a Fellow of the American College of Healthcare Executives.
He is the author or co-author of over 100 papers published in peer-reviewed professional journals. He served as an oral examiner for the American Board of Obstetrics and Gynecology (ABOG) for 19 years. He served as Chairman of the Connecticut Hospital Association’s Quality Committee and was a member of its Executive Committee and Board of Directors. He currently serves on the Board of Trustees of the University of Saint Joseph. He was awarded the 2020 Regent’s Senior Careerist Award by the Connecticut Association of Healthcare Executives.








Comment will held for moderation